Unlocking Medical Records: Essential Tips for Attorneys
Buried within pages of medical records are the details that can make or break your case. You have been sent thousands of pages of medical jargon, disorganized notes, duplicated reports, and cryptic abbreviations. How do you find the critical details needed for your case?
Basics of Medical Records
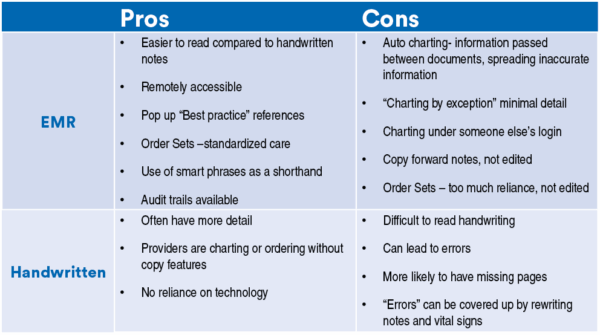
First, an understanding of medical records is important. Medical records are in the format of Electronic Medical Records (EMR), handwritten notes, or a mixture of the two forms. Below are a few of the pros and cons of each type.
- Here is a list of the parts of the medical record with a brief description of what each contains:
- Demographics – general patient information
- Consents – signed forms required for admission and procedures
- History and Physical (H&P) – medical history, physical exam on admission
- Progress Notes – daily doctors notes
- Nursing Notes – assessment every shift, changes in assessment
- Flow Sheets – vital signs, intake/output, IV/drains/line assessments, safety, blood administration, etc.
- Interdisciplinary –therapies, social work, dietary, etc.
- Consults – specialists, surgical
- Lab Results – blood work, cultures
- Imaging – Xray, MRI, CT
- Medications –the medication administration record (MAR) lists all medication given during a stay, doses, and routes
- Discharge – paperwork documenting the preparation for discharge, teaching, or safety measures
- Other – Scanned Transport records, CODE sheet, etc.
Records to Obtain
Wording a request for medical records is crucial. Typically the records are copied or transferred electronically by staff from the IT department. Parts of the records are often missing including imaging reports, scanned documents, and data from messaging platforms such as Inbox and patient portals.
Other documentation that can be helpful to obtain are policies, procedures and incident reports. While there are basic standards of care for nurses and medical providers, policies and procedures give the specific standard for the facility or unit. Incident reports are a written account of any unexpected incident such as a fall or a medication error. Incident reports are under the umbrella of Quality Assurance and designed as a tool to improve healthcare. However, in some instances, an incident report can be discoverable and can be beneficial if the incident is missing from the medical record.
Another source of documentation that can be obtained with an EMR record is an audit trail. It shows the footprint behind the medical record including changes, deletions, and where and when staff logged into computers. Audit trails can be used to refute or corroborate testimony from healthcare professionals. For example, if a provider states in deposition that they were at the patient’s bedside ordering treatments, an audit trail might show that the provider was at home or in another office at the time. Audit trail records may be sent in PDF format; however, it is beneficial to request them in Excel format because the information can be sorted and filtered for easier review. When requesting audit trails, the wording should include “PDF format with the sort box or AutoFilter options checked to allow sorting.”
Reviewing Medical Records
When reviewing medical records it is beneficial to start with a chronology. Medical records should be sorted according to time and not by section. For example, when reviewing an incident on a specific day, it is helpful to have the vital signs, nursing notes, physician notes, testing, and treatment for that day all in one place. This will show the flow of treatment. There is a pattern to medical care: a health concern, an assessment, testing, diagnosis, treatment, reassessment, and then repeat if the treatment did not resolve the problem. Having the documents sorted by time will facilitate finding the patterns and what is missing.
Common Pitfalls
There are common pitfalls to avoid when reviewing medical records. Hyper-fixating on a specific issue leads to missing information. It is essential to review every page and look for gaps in time. There are standards for frequency of vital signs and assessments and a standard time to evaluate high-risk situations such as stroke, heart attack and emergency cesarean section.
Be aware that values that are highlighted red may not be important. Vital signs and laboratory results differ between age groups, diagnoses and certain medications. When these values are either highlighted red or have a “high” or “low” notation, they may actually be appropriate for that patient. Knowing the correct values for a patient is critical to the analysis of the medical record.
Thinking outside of the box may provide more information or clues to missing documentation. Records for billing or health insurance can provide names of other physicians and visits a client had. A nursing care plan or Kardex may have information about concerns for the client’s care that were not addressed in the medical record. Scanned documents and outside diagnostic testing results may include vital information and are often missing from the medical record. If there are no scanned documents, a thorough review of the physician orders will show if outside testing was ordered and nursing notes may state the test was done.
Medical abbreviations are not always consistent or standardized. One abbreviation can mean two things and must be reviewed in the setting of context, for example “BS” is breath sounds and bowel sounds and “PROM” is passive range of motion and premature rupture of membranes. For resources on medical terminology and abbreviations, check the hospital pre-approved list, medical or nursing schools, and published books or pamphlets. Use caution with online searches, as previously stated, there are numerous medical abbreviations, and they are easily confused.
Red Flags
There are certain elements in medical records that are red flags. They often show when an error occurred, if there is missing documentation, or potential tampering of the records. Time gaps in care are red flags that something is missing.
Any reference to an event that should have a corresponding note, such as a code, procedure, or surgery, but a note is not in the records, is a critical red flag. If there is little or no documentation for a significant event, then something is missing. Another red flag is when there are documented changes in the patient’s condition, and a follow-up is not addressed in the record.
By navigating medical records effectively, attorneys can decode critical information to build stronger cases. The ability to interpret and leverage medical records is vital for attorneys to not only enhance their practice but also make strides toward achieving justice for their clients.